Wilfredo Santa Gómez, MD
Child, Adults and Adolescents Psychiatrist HarvardMedical School Ex Faculty Appointed Fellow
The COVID-19 pandemic has had a significant impact on the mental health of people worldwide. The fact that depression is one of the most common mental disorders globally. affecting over 264 million people of all ages worldwide, with a consistent prevalence fluctuating around 5% of the global population. Since I am focusing particularly on the young adults, children and adolescents groups of Puerto Ricans, it is important to clarify that prevalence of depression varies across countries and regions, with higher rates observed in some parts of the world compared to others.
Dozens of studies has demonstrated that rates of depression tend to vary based on factors such as cultural, environmental, and socio-economic differences. While depression can affect individuals in any part of the world, studies indicate that regions like North America, Europe, and Australia have higher rates compared to other parts of the world.
Risk Factors contributing to the development of depression include biological, psychological, and social factors. But in general risk factors for depression has been grouped as follows:
1. Genetics: A family history of depression or other mental health conditions can increase an individual’s susceptibility to developing depression.
2. Brain chemistry: Imbalances in certain neurotransmitters, such as serotonin and dopamine, can contribute to the onset of depression.
3. Life events: Traumatic experiences, loss of loved ones, relationship problems, work-related stress, or financial difficulties can trigger or exacerbate depressive symptoms.
4. Chronic medical conditions: People living with chronic illnesses like cancer, diabetes, heart disease, or chronic pain may be at a higher risk of developing depression.
5. Substance abuse: Drug or alcohol abuse can lead to depression or worsen existing symptoms.
6. Gender: Females tend to experience depression at higher rates than males, although this difference may be partly due to underreporting in men.
Some impacting figures like suicide rates are directly link to depression and they significantly increased between 2020 and 2021 for males aged 15–24, 25–44, 65–74, and 75 and over, from 2020 to 2021, suicide rates increased significantly for non-Hispanic Black (subsequently, Black) and non-Hispanic White (subsequently, White) females.From 2020 to 2021, suicide rates increased significantly for non-Hispanic American Indian or Alaska Native, Black, and White males.
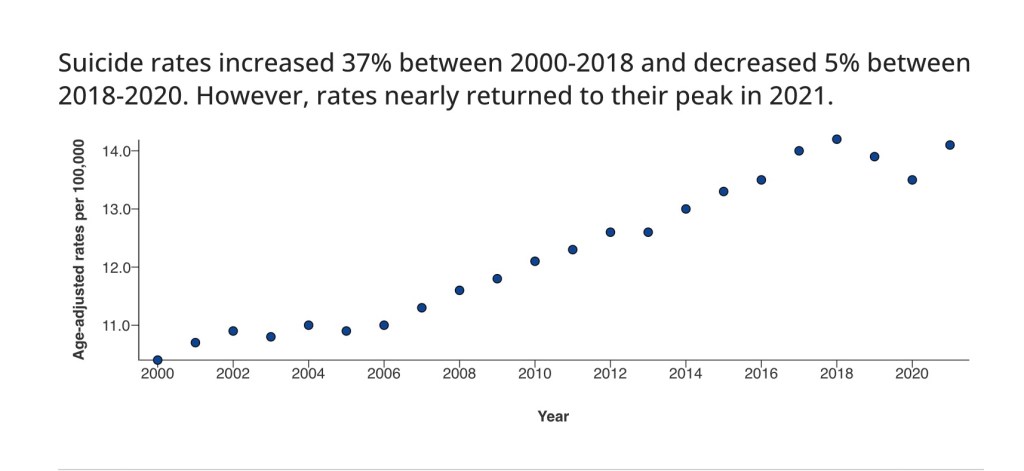
We all need to be alert first by learning more about the multiple faces of depression, and by learning to read the many different messages that different people with depression are transmitting to others, sometimes even without recognizing that they are clinically depress. Special concern on people experiencing depresión is their elevated risk for suicide. According to the information on suicide reported on CDC’s website, suicide is one of the leading causes of death in the United States. Data from 2001–2021 available on that website on CDC showed an increased from between 2001 (10.7) and 2018 (14.2), the age-adjusted suicide rate declined for 2 years through 2020 (13.5), and then increased to 14.1 in 2021. It is also reported on the CDC website that female suicide rates varied over the period, and the observed increase between 2020 and 2021 was significant only for those aged 75 and over.
Learning about early detection of depression, familiarizing yourself with those signs and symptoms, becomes eaven more important when it is well known that a large group of people suffering from chronic severe and recurrent forms of mood disorder are known to have experienced their first episode of illness early in life. The clinical presentation of depression at this stage of life can be complex and unusual and is often complicated by personality issues, substance use disorders, and other concomitant individual or extended family crisis (divorce, unemployment, college education expenses, etc.). And on top of everything else, we are dealing now with the sudden emergence of a unique top stressor, the pandemic of Covid-19 coronavirus.
On the other hand you have additional proof on the impact of early depression on adulthood by many widely accepted studies showing this fact as an indicator of susceptibility, proven by many studies like the well known classical study of Maudsley long-term follow-up of child and adolescent depression patients (Reference Fombonne,Wostear and Cooper-Fombonne et al, 2001), they followed 149 participants for over a 20 years period and found that 62% of them experienced recurrence major depression episodes and also 44% of them had at least one suicidal attempt episode (Reference Fombonne,Wostear and Cooper-Fombonne et al, 2001)
Another study demonstrated that patients who had suffered from young adult early depression experienced elevated levels of social dysfunction and higher health services utilisation than the general adult population did (Reference Knapp, McCrone and Fombonne- knapp et al, 2002). We also know the role play by genetics, since un doubly family and adoption studies consistently have
demonstrated that depression runs in families.
The pandemic des acceleration effect that impacted all aspects of our life that lasted for more that a year, still an ongoing event, causing disruptions in all aspects of our daily functioning, like in children and young adults education, health, social an family life, deterioration in quality and frequency of normal communication, predominantly dominated by feelings of anxiety, fear and uncertainty about the future. Losses of all types, including the death of significant ones, it all impacted many generations involved in the Covid-19 pandemic.
The pandemia needs to be consider as an amplifier of the well known and studied epidemiological depression precipitant factors, imposing limitations on communication, social interactions, disrupting the healthy flow of information, therefore without doubts acting as a precipitant factors, adding confusion, feelings of isolation, anxiety, and loss of purpose, to the panorama. All this facts contributed by acting as an amplification effect and will required to be considered as strong determinant indicators of an elevated risk for this entire population of developing a Major Depressive episode during pandemic and post pandemic time. Readers will benefit from learning of factual evidence that not only negative life events can precipitate depression, events considered positive by the general population, like finishing High School or college may equally trigger a life crisis and depression.
It is well known, intuitively and by studies that people with depression are more prone to produce stressful events, and it is also known that if they are carrying a higher genetic loading for affective disorder, it will make them more prone to suffer a major depression episode after a stressful life event, represented in our case by the pandemic, than those with low genetic loading but doesn’t necessarily need to be present. (Reference Silberg, Rutter and Neale et al, 2001).
Summarizing , it is a fact that traumatic experiences can be disruptive by interfering with our normal emotional and psychological development, as ocurre with abused neglected individuals that show lot of difficulties in achieving the necessary resolution of adolescence and early adulthood conflictual issues, sufficiently for them to be able to make a healthy and more successful entrance to the next adulthood challenging scenario.
But unexplainably, other similarly catastrophic events like ground cero destructive hurricanes (represented by Puerto Rico Hurricane Maria), or destructive force earthquakes (also in Puerto Rico months after Hurricane Maria) and by other catastrophic not so clearly foreseen events like a major government financial collapses (also represented by countries bankruptcies actually happening in Puerto Rico), or even bigger, the devastating not only less foreseen but time camouflaged ignored catastrophic event, of the longest duration of all reported in the history, again exemplified by a country forced occupation by another country, (represented by the 530 years occupation of Puerto Rico first Spain afterwards USA) , also happening in Ucrania.

Additionally, it has also been studied that not all abused individuals showed psychopathological disorders during adulthood, demonstrating that the susceptibility to stress has a stronger genetic make-up correlation and become more visible and even stronger proved by the resilience fostered and seeing on residents in occupied territories ( 530 years continuous-occupation) like Puerto Rico, where its habitants had suffered and gone trough five major recent catastrophic PTSD generator events, amongst them hurricane Maria (a ground cero devastating event), that forced the population to become familiar with the term “resilience”.

In Puerto Rico the entire population surviving all this events, had shown to be a unique case, here the kind of “unadulterated pure deeply ingrained resilience” not seen before in history, is signaling us out as what could be a distinct and very excellent scientific opportunity to become another strong proof of individuals supporting recent work on depression which confirmed that genetic factors play an important role in determining our susceptibility to environmental stress, although this study was performed only in adolescent girls, researchers should consider the possibility of moving to Puerto Rico to run a study on this unique population that has been impacted in a short period of time by so many disasters, where the term resiliency has become emblematically over used, (Reference Silberg, Rutter and NealeSilberg et al, 2001).
The post pandemic panorama, painted with economic instability, job losses, and financial pressures, directly affected young adults starting their careers, stressors that also contributed to the development or exacerbation of depression among this demographic.To worsen the situation, the reduced access to mental health services during the pandemic has posed a barrier for young adults seeking professional help. The closure of counseling centers, limitations on in-person therapy sessions, and the shift towards virtual platforms have made it more difficult for individuals to access the support they need, leading to increased distress and potentially worsening depression.

It is important to mention that while some young adults may experience increased levels of depression, many others may develop resilience and find ways to cope effectively with the challenges brought by the pandemic. Factors such as personal resiliency, strong support systems, and access to mental health resources can play a significant role in mitigating the negative effects on mental health.
What needs to be done? A group as well as an individua approach are part of the requirements in order to address the mental health needs of young adults during and after the pandemic, it is crucial to prioritize accessible and affordable mental health services, a team approach and reach out attitude are absolutely necessary for promoting awareness campaigns to reduce stigma surrounding mental health, and ensure that educational institutions and workplaces provide appropriate support and resources.
All available studies has shown that onset of depression in adolescence or young adulthood represents a severe form of affective disorder associated with poor long-term outcomes. It often arises in families where multiple first- and second-degree relatives have a mood disorder and most of the time complicated by substance use disorder.
Also the planificación and design of and array of ways to help fostering strong and healthy social connections, encouraging healthy coping mechanisms, and promoting self-care practices can also help young adults navigate these uncertain times and mitigate the impact covid-19 pandemic left in form of depression in our young population.
Other useful actions that you my try, only if you feel confortable doing them, if not , call for help:
- Urge the person to stay with treatment. If someone is in treatment for depression, help them remember to take prescriptions and keep appointments.
- Be willing to listen. Let them know that you want to learn how they feel. When they want to talk, listen carefully. But don’t give advice or opinions and don’t judge them. Just listening just being understanding can be a powerful healing tools.
- Give positive reinforcement. People with depression may judge themselves harshly and find fault with everything they do. Remind them about their positive qualities and how much they mean to you and others.
- Offer help. A person may not be able to take care of certain tasks well. Suggest specific tasks you’d be willing to do. Also, ask if you can take on a particular task.Help make their life less stressful.
- Creating a regular routine may help a person with depression feel more in control. Offer to make a schedule for meals, medicine, physical activity, social support and sleep, and help organize household chores.
- Find helpful organizations. Many organizations offer support groups, counseling and other services for depression. For example, the National Alliance on Mental Illness, as well as employee assistance programs and many faith-based organizations, offer help for mental health concerns.
- Urge them to take an active part in their faith, if faith is a part of their life. For many people, faith is an important part of recovery from depression — whether it’s taking part in an organized religious community or personal spiritual beliefs and practices.
- Urge the person to take self-care steps. That includes eating healthy meals, getting the right amount of sleep and being physically active.
- Make plans together. Ask the person to join you on a walk, see a movie with you, or work with you on a hobby or other activity they enjoyed before.
- But don’t try to force them into doing something.
- It is a globally known fact that when someone is depressed it is mandatory to ask the person directly about presence of suicidal feelings or thoughts, at present or at some point in the past.
Always consider all signs of suicidal behavior seriously and act immediately as previously indicated. (Must read CDC website guidelines about how to ask),
Here I wrote some of the general guidelines recommended by mental health professionals worlwide that you my find as well on the CDC website:
Tell the person why you’re worried. Ask if they’re thinking about suicide or have a plan for how to do it. Having a plan means it’s more likely they’ll attempt suicide. Seek help. Contact the person’s health care provider, mental health provider or another health care professional. Let other family members or close friends know what is going on. If you detect any sings of suicide like this ones:
Then you may:
- Check and write down all crisis hot lines numbers of your lical area, including suicide risk hot lines.
- Contact a suicide hotline.
- Ask for advice and what resources are in your area. Or urge the person at risk to contact a hotline for counseling.
- In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline. It’s available 24 hours a day, every day. Or use the Lifeline Chat. Services are free and private.
- U.S. veterans or service members who are in crisis can call 988 and then press “1” for the Veterans Crisis Line. Or text 838255. Or chat online.
The Suicide & Crisis Lifeline in the U.S. has a Spanish-language phone line at 1-888-628-9454 (toll-free).- Make sure the person is safe. If possible, get rid of things that could be used to attempt suicide.
- For example, remove or lock up firearms, other weapons and medicines ( In USA, in 50% of all violent death last year a personal firearm was involved)
- Call 911 or your local emergency number right away if a person could harm themselves or attempt suicide.
- Make sure someone stays with the person at all times.
- Stay alert for warning signs of suicide.
- common warning signs of suicide or suicidal thoughts:
Show support:
- Remember that you should not blame yourself for being depress or for having any affective disorder diagnosis.depression isn’t anyone’s fault. You can’t fix someone’s depression, but your support and understanding can help. Just learn to listen!
keep yourself from burning out, Ask for help:
Caring for someone with depression isn’t easy. Ask other relatives or friends to help. Tell them what you need.
Take steps to stay healthy. Find time for yourself. Do what you enjoy, stay physically active, check in with friends and renew your spirit.
Be patient. Depression symptoms improve with treatment, but it can take time. Finding the best treatment may require trying more than one type of medicine or treatment approach. For some people, symptoms quickly improve after starting treatment. For others, it will take longer..
Never forget to always consult a hotline or a mental health profesional.